Now, don't get me wrong. Taking medication is NOT the ONLY step you should be taking to treat your or your child's ADHD. Diet and parenting have to be reworked. Educational and behavioral supports need to be put into place and "coaching" or other mental-health/behavioral interventions should be considered. This is a very big deal and requires serious effort.
Don't ever, ever, ever think that popping a pill is the end of it. Most children with ADHD have some type of processing disorder that erupts in academic problems and behavioral challenges. I've had parents come to me years after their child has been diagnosed and treated for ADHD only to report continuing academic decline and behavioral escalation. It is intensely associated with dyslexia, language-related learning disabilities and all kinds of learning misery. If your child is being evaluated for learning problems that you suspect are related to ADHD, you MUST evaluate for slow processing speed and memory deficits. Trust me. "Something else" is lurking there and it's the kind of "stuff" that can sabotage even the most diligent student. At times, treating the ADHD reveals underlying anxiety, depression or bipolar disorder.
The symptoms of ADHD overlap many other disorders. It's important to get it right. The most challenging question to answer is this one: "Is this ADHD or is it something else masquerading as ADHD or is it ADHD + something else?"
Years ago, parents referred their teenage son to me and the final diagnosis was schizophrenia. It was difficult for the young man to pay attention when voices were telling him to do "unspeakable things". The various forms of ADHD are associated with:
- Intermittent explosive disorder
- Stereotypical movement disorder (tics, Tourette's Disorder)
- Specific learning disorders
- Reactive attachment disorder
- Anxiety disorders
- Intellectual disabilities (formerly called mental retardation)
- Autism spectrum disorder
- Depressive disorders
- Bipolar disorders
- Disruptive mood dysregulation disorder
- Substance use disorders
- Personality disorders
- Psychotic disorders
- Medication-induced symptoms of ADHD
- Neurocognitive disorders
- Oppositional defiant disorder
A diagnosis of ADHD can still be assigned to these conditions, but clearly, it's not the only issue at hand. All symptoms have to be evaluated and addressed.
Parents often ask about the difference between ADD and ADHD. The Diagnostic and Statistical Manual was first published in 1952. It wasn't until the 2nd Edition (1968) that any type of ADHD-ish disorder was identified. The "hyperkinetic reaction of childhood" referenced having a short attention span and hyperactivity/restlessness.
By the time the 3rd Edition of the DSM came along in 1980, the disorder was changed to Attention Deficit Disorder (ADD) which respected the fact that attentional problems could be separate from impulse-control problems. This label represented an essential shift in the definition and focused primarily on problems related to inattention versus hyperactivity/impulsivity. To differentiate between the two subtypes in the DSM-III, the disorder was described as ADD/H (with hyperactivity) and ADD W/O (without hyperactivity, essentially the inattentive type).
The DSM-III was revised in 1987 (DSM-III/R) the disorder was called Attention-Deficit/Hyperactivity Disorder and did away with the subtypes. Yep, apparently, you couldn't have ADHD without a whole lotta "H". You weren't allow to have only the inattentive type which, frankly, kept many girls from being diagnosed because we see the inattentive type associated with female neurology.
Then, the research kicked in. It was proven that a person could have inattention without hyperactivity and off we go again! The DSM-IV (1994) kept the name ADHD. Two categories were created for the inattentive symptoms and the hyperactive/impulsive symptoms which were described 3 subtypes: ADHD, Primarily Inattentive Type; ADHD, Primarily Hyperactive/impulsive Type; and ADHD, Combined Type.
The DSM-5 was published in 2013 and offers the following ADHD diagnoses:
- Predominantly Inattentive Presentation (ADD)
- Predominantly Hyperactive-Impulsive Presentation (ADHD)
- Combined Presentation
All three, diagnostically, can be rated as Mild, Moderate or Severe or "In Partial Remission". The diagnosis cannot be made if the symptoms result from an illness or medication reaction/drug abuse.
Taken directly from the DSM-5 (starting on page 59), the diagnostic criteria are as follows:
A. A persistent pattern of inattention and/or hyperactivity-impulsivity that interferes with functioning or development, as characterized by (1) and/or (2):
1. Inattention: Six (or more) of the following symptoms have persisted for at least 6 months to a degree that is inconsistent with developmental level and that negatively impacts directly on social and academic/occupational activities:
NOTE: The symptoms are not solely a manifestation of oppositional behavior, defiant, hostility, or failure to understand tasks or instructions. For older adolescents and adults (age 17 or older), at least five symptoms are required.
a. Often fails to give close attention to details or makes careless mistakes in schoolwork, at work, or during other activities (e.g., overlooks or misses details, work is inaccurate).
b. Often has difficulty sustaining attention in tasks or play activities (e.g., has difficulty remaining focuses during lectures, conversations or lengthy reading).
c. Often does not seem to listen when spoken to directly (e.g., mind seems elsewhere, even in the absence of any obvious distraction).
d. Often does not follow through on instructions and fails to finish schoolwork, chores, or duties in the workplace (e.g., starts tasks but quickly loses focus and is easily sidetracked).
e. Often has difficulty organizing tasks and activities (e.g., difficulty managing sequential tasks; difficulty keeping materials and belongings in order; messy, disorganized work; has poor time management; fails to meet deadlines).
f. Often avoids, dislikes, or is reluctant to engage in tasks that require sustained mental effort (e.g., schoolwork or homework; for older adolescents and adults, preparing reports, completing forms, reviewing lengthy papers).
g. Often loses things necessary for tasks or activities (e.g., school materials, pencils, books, tools, wallets, keys, paperwork, eyeglasses, mobile telephones).
h. Is often easily distracted by extraneous stimuli (for adolescents and adults, may include unrelated thoughts).
i. Is often forgetful in daily activities (e.g., doing chores, running errands; for older adolescents and adults, returning calls, paying bills, keeping appointments).
2. Hyperactivity and impulsivity: Six (or more) of the following symptoms have persisted for at least 6 months to a degree that is inconsistent with developmental level and that negatively impacts directly on social and academic/occupational activities:
NOTE: The symptoms are not solely a manifestation of oppositional behavior, defiance, hostility, or a failure to understand tasks or instructions. For older adolescents and adults (age 17 and older), at least five symptoms are required.
a. Often fidgets with or taps hands or feet or squirms in seat.
b. Often leaves seat in situations when remaining seated is expected (e.g., leaves his or her place in the classroom, in the office or other workplace, or in other situations that require remaining in place).
c. Often runs about or climbs in situations where it is inappropriate. (Note: In adolescents or adults, may be limited to feeling restless).
d. Often unable to play or engage in leisure activities quietly.
e. Is often "on the go", acting as if "driven by a motor" (e.g., is unable to be or uncomfortable being still for extended time, as in restaurants, meetings;
may be experienced by others as being restless or difficult to keep up with).
f. Often talks excessively.
g. Often blurts out an answer before a question has been completed (e.g.,completes people's sentences; cannot wait for turn in conversation).
h. Often has difficulty waiting his or her turn (e.g.,while waiting in line).
i. Often interrupts or intrudes on others (e.g., butts into conversations, games, or activities; may start using other people's things without asking or receiving permission; for adolescents and adults; may intrude into or take over what others are doing).
B. Several inattentive or hyperactive-impulsive symptoms were presents prior to age 12 years.
C. Several inattentive or hyperactive-impulsive symptoms are presents in two or more settings (e.g., at home, school, or work; with friends or relative; in other activities.
D. There is clear evidence that the symptoms interfere with or reduce the quality of, social, academic, or occupational functioning.
E. The symptoms do not occur exclusively during the course of schizophrenia or another psychotic disorder and are not better explained by another mental disorder (e.g., mood disorder, anxiety disorder, dissociative disorder, personality disorder, substance intoxication or withdrawal).
If A1 (inattention) and A2 (hyperactivity-impulsivity) are met for the past 6 months, you've got the Combined Presentation.
If A1 (inattention is met), but A2 (hyperactivity-impulsivity) is not met for the past 6 months, you've got the Predominantly Inattentive Presentation.
If A2 (hyperactivity-impulsivity) is met and A1 (inattention) is not met for the past 6 month, you've got Predominantly Hyperactive/Impulsive Presentation.
The disorder can be mild, moderate or severe and even in "partial remission" which means: "When full criteria were previously met, fewer than the full criteria have been met for the past 6 months, and the symptoms still result in impairment in social, academic or occupational functioning."
Diagnostic Features, Associated Features Supporting Diagnosis, Prevalence, Development and Course, Risk and Prognostic Factors, Culture-Related Diagnostic Issues, Gender-Related Diagnostic Issues, Functioning Consequences of Attention-Deficit/Hyperactivity Disorder, Differential Diagnosis and Comorbidity are sections offered to more fully discuss the disorder.
The DSM-5 reports that ADHD occurs "in most cultures in about 5% of children and about 2.4% of adults".
Additional diagnoses include "Other Specific Attention-Deficit/Hyperactivity Disorder" and "Unspecified Attention-Deficit/Hyperactivity Disorder" are used when the symptoms "cause clinically significant distress or impairment in social, occupational or other important areas of functioning predominant but do not meet the full criteria for attention-deficit/hyperactivity disorder or any of the disorders in the neurodevelopmental disorders diagnostic class".
EXTREME care must be taken when evaluating children under the age of 4 because there is much greater variability in their development than in older kids. This means that a 4 year old might look ADHD, but be more excitable and "busy" than other 4 years old, but is not diagnosable.
Additionally, diagnosing adults requires great care. It's important not to rely solely on an adult's memory for their specific symptoms. Gather data from others who knew them when they were younger. Evaluate school records if they are available. Many adults with ADHD also suffer from diagnosable levels of anxiety and depression because of the cumulative effects of life's struggles. It's important to make a correct diagnosis. The untreated ADHD might be responsible for the anxiety and depression, so treating the ADHD first may be the most effective step. Once the data is gathered, I refer my adult clients to a psychiatrist to rule out substance abuse and other disorders which may mask as ADHD. Clinicians need to be mindful of those adults (and older teens) who are "shopping" for a prescription.
A final note. I've seen this super bright kids who are very, very busy. Don't misdiagnose them! They could fall into the category of Gifted Overexcitable. They're just smart and their minds are full of ideas! Be careful.
Many of you with a form of ADHD yourself, parent a child with ADHD or teach children with ADHD are likely to agree that Daniel Amen's description of the 7 types of ADHD more meaningfully describe the reality of the disorder. There are those who disagree with his approach and I'm not the kind of clinician who is completely sold on anything, but collecting information is critical to helping us understand this very complex condition.
I took this information from a variety of his writings I have in my office as well as from his website in order to present very brief descriptions of his categories. I've added some of my own comments. Dr. Amen labels all of his ADHD types as ADD.
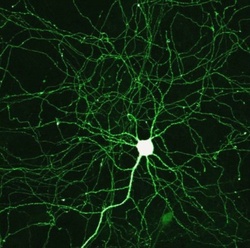 The magical, mystical, miraculous neuron.
The magical, mystical, miraculous neuron.
2. Overfocused ADD: Can pay attention, but can't shift attention. World just passes by them.
3. Inattentive ADD: Introverts, limited attention span unless interested, easily distracted, minimal hyperactivity/impulsivity, can be disorganized and operate on the "fear factor" of waiting until the last minute to do things, time management issues and misjudging the complexity of a task and the amount of time it will take to complete it.
4. Temporal Lobe ADD: Temporal lobes (below the temples and behind the eyes) are involved in controlling temper and stabilizing mood. Characterized by aggression, mood instability, learning problems and difficulties with memory. [Beware! Stimulants worsen symptoms.]
5. Limbic ADD: ADD and mood disorders/depression are the causes of this type of ADHD; sufferers experience low-levels of depression along with chronic ADD symptoms.
6. Ring of Fire ADD: Excessive activity in nearly all parts of the brain. Aggressive, intense, inflexible, rigid, extreme moodiness, outbursts of temper, oppositional, non-stop/fast thoughts, sensitivity to sound and light.
7. Anxious ADD: Anxiety, nervousness, physical tension, pessimistic, trouble with timed activities or working under the pressure of time, fear of public speaking along with other ADD symptoms.
These various forms of ADD are treated with medications, supplements, exercise and diet as well as behavioral/parenting interventions and therapies.
I arrange to conduct two "blind" observations and sit in the classroom on two different days and two different times of the day. The observation is "blind" because my client does not know me. [It's my experience, however, that my client, despite not knowing me or why I am there, turns around and looks at me frequently!] I collect data from teachers using the Conners 3 Rating Scales (Long form) and a teacher feedback form that I created that asks teachers to offer comments about the student's classroom participation, test performance, homework performance and strengths and weaknesses. .
I write up the information and meet with parents. If there is enough evidence to suggest that an ADHD diagnosis is viable, I ask them to complete a very extensive (36 pages!) developmental history and a set of forms including their version of the Conners 3 (Long form), a Behavior Assessment System for Children-2nd Edition scale and if their child is 11 years or older, the Behavior Rating Inventory of Executive Functioning.
I meet with my client and conduct an interview. If my client is 8 years and older, I work through the Conners Self-Report Scale (Long form) with them.
I meet with parents and discuss the results and the plan. If a diagnosis is made, I meet with my client and explain the "brain stuff" about ADHD so they can discriminate between their neurology and their "personhood". I don't want them to feel damaged or defective in any way. I can't remember the last time a child/teen was upset with the news. They appreciate knowing "what's going on" and that there is a reason for all of their distress.
There is a Conners Early Childhood version that is for children who are 2 years, 0 months through 6 years, 11 months old. It is very thorough and evaluates the following areas:
- Inattention/Hyperactivity
- Defiant/Aggressive Behaviors
- Social Functioning/Atypical Behaviors
- Anxiety
- Mood and Affect
- Physical Symptoms
- Adaptive Skills
- Communication
- Motor Skills
- Play
- Pre-Academic/Cognitive
I have confidence in this instrument because it looks very carefully at the child's global functioning.

A QEEG is a quantitative electroenceph-alogram study of the electrical activity in the brain. It is commonly called "brain mapping" and is often the diagnostic process before neurofeedback treatment begins. It is also used as part of the psychosocial approach of diagnosing ADHD.
LENS, or Low Energy Neurofeedback System, is generally not used to treat any specific condition, but "optimizes brain functioning" and regulating moods. It has proven to be effective in the treatment of ADHD.

Resources include:
Edward Hallowell and John Ratey's Driven to Distraction regarding ADHD in adults. It also addresses childhood ADHD, but was a groundbreaking discussion for adults. Has a great checklist for adult ADHD. Dr. Hallowell has ADHD and this book was the first to document that ADHD in adults is a discrete disorder and is not always "just" an artifact of anxiety or depression.
Children with Attention-Deficit/Hyperactivity Disorder (CHADD) is a nation-wide organization with information and resources regarding ADHD in all persons. This subscription comes with a subscription to Attention!, a monthly magazine. On their website, you can find out where your local chapter meets. Go to the meetings to hear local experts who can give you guidance.
I like the ADD WareHouse for everything under the sun that is related to ADHD. It's where I found Sari Solder's Book, Women with Attention-Deficit Disorder. It's a unique perspective that really helps my female ADHD clients.
ADDitude magazine is my hands-down favorite. I subscribe to their alerts and get great info nearly daily, but the amount of "stuff" they send out can be overwhelming, so start out with the magazine to get yourself going.
I consider the various forms of ADHD to be one of the most destructive disorders I diagnose. I've seen all its ugly mess including the Oppositional Defiant-Conduct Disorder-Antisocial Personality Disorder continuum. The cost of destruction is indescribable, but you don't have to go there. Work toward the highest quality of life you and your family can have. Stay calm and carry on!
Claudia
Join me on Facebook at Dr. Claudia McCulloch
At drclaudia.net, click on the "Ask Me" button and submit a question.